Sedation of Pediatric Patients during Echocardiogram: Review Article
Ashly Diaz*
Department of Pathology, Odense University Hospital, Odense, Denmark
- *Corresponding Author:
- Ashly Diaz
Department of Pathology, Odense University Hospital, Odense, Denmark
Tel: 8132984895
E-mail: diazashley20@gmail.com
Received date: April 06, 2023, Manuscript No. IPIPC-23-16275; Editor assigned date: April 10, 2023, PreQC No. IPIPC-23-16275 (PQ); Reviewed date: April 25, 2023, QC No. IPIPC-23-16275; Revised date: June 06, 2023, Manuscript No. IPIPC-23-16275 (R); Published date: June 14, 2023, DOI: 10.36648/IPIPC.7.03.261
Citation: Diaz A (2023) Sedation of Pediatric Patients during Echocardiogram: Review Article. Insigh Pediatr Card Vol:7 No:3
Abstract
Echocardiography is a noninvasive ultrasonographic tool used to examine the heart. It is useful for analyzing the anatomy, physiology and functions of the heart; and is considered essential for diagnosing heart disease and defects in infants and children. However, conducting a proper echocardiogram on younger patients can be a considerable challenge due to their crying, screaming, and persistent resistance to sitting still. The objective of this review article is to compare the different sedative drugs used in pediatric patients to achieve cooperation during an echocardiogram. There are also other more traditional methods of minimizing cooperation problems such as feeding and distracting the patient, which will be discussed briefly to help evaluate the difference in diagnostic errors in pediatric patients that are sedated versus not.
Keywords
Echocardiogram; Pediatrics; Sedation; Diagnostic error; Anatomy; Physiology
Introduction
For the evaluation of children with congenital and acquired heart diseases, Transthoracic Echocardiography (TTE) is the most efficient imaging modality. A TTE can provide the structural, functional, and postural defects that cause heart disease in pediatric patients [1]. It is important to get reliable echocardiogram results because most management decisions are based on echo findings rather than invasive procedures like cardiac catheterizations. A cooperative patient is essential for a thorough and error-free echocardiogram. It can be difficult to achieve optimal results in young children, as with other pediatric procedures. Therefore, many centers now routinely use sedatives to perform echocardiograms in young children. Some of the different types of sedatives used in pediatric patients include anxiolytic drugs, hypnotic drugs, analgesic drugs, and in rare cases opioid agonists for pain management [2]. In a normal echocardiogram, midazolam is sufficient, whereas in a transthoracic echocardiogram more powerful immobilizing drugs like chloral hydrate is preffered. Other sedatives commonly used in children include dexmedetomidine, phenobarbital and pentobarbital. There are, however, risks associated with sedating young children.
Literature Review
Sedative drugs used in pediatric patients
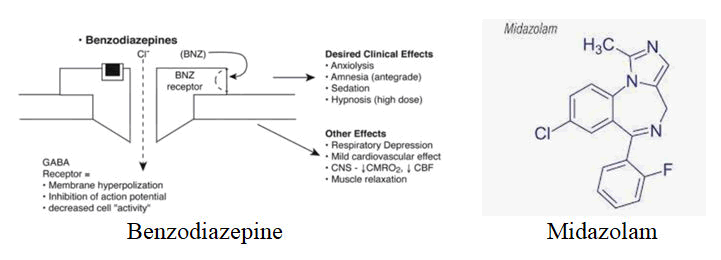
Midazolam: Midazolam is a benzodiazepine that falls under the anxiolytic drug category as it makes children more manageable. It increases Gamma Aminobutyric Acid (GABA) in the brain and is frequently used for sedation in the pediatric population because it is short acting and has quick onset properties [3]. By increasing GABA in the brain, it enhances chloride flux resulting in membrane hyperpolarization and inhibition of action potential, and thus decreased cell activity [4]. The desired clinical effects are muscle relaxation, antegrade amnesia, sedation and in high doses hypnosis. The adverse effects it can cause are respiratory depression, a mild decrease in cardiac output and decreased oxygen consumption by the brain, but rarely occur when given alone and normally happens when given in conjunction with other sedatives [5]. Paradoxical reactions such as inconsolable crying and aggressive behavior although rare can occur, and should be reversed with flumazenil, a GABA receptor antagonist. It is frequently used in conjunction with other sedatives to achieve optimal results, as it is not always reliable when given alone in procedures requiring more immobilization. It’s ability to be administered orally, via IV, rectally, and intranasally is also beneficial [6]. Nonetheless, midazolam has variable metabolism when administered orally making dosing difficult.
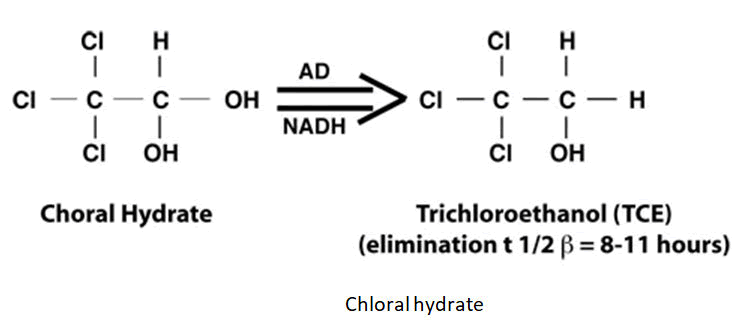
Chloral hydrate: Chloral hydrate is a hypnotic drug that is most widely used in sedation of pediatric patients here in India, and generally considered safe and effective. It is a 2,2,2-trichloroacetaldehyde, that is metabolized in the liver by alcohol dehydrogenase into trichloroethanol, the active metabolite. It is highly effective in non-painful procedures like TTEs, CTs, and MRIs which demand complete immobilization. It can be administered either oral or rectal and dosed at 50-75 mg/kg. It has an induction time of 15-25 minutes, and a recovery time of 60-120 minutes. For these reasons it is no longer recommended in many parts of the world [7]. Some of the common adverse effects include oxygen desaturation, cardiac arrhythmias, vomiting, and agitation.
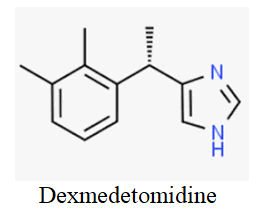
Dexmedetomidine: Dexmedetomidine is a newer beta-2 adrenoreceptor agonist that is odorless, colorless, and tasteless. It is formulated in a concentration of 100 μg/ml and administered intravenously at a dose of 2.5-3.0 μg/kg. It can also be administered intranasally at the same dosage. When given via buccal the dosage is 3-4 μg/kg, just slightly higher. It has a slower onset than other sedatives, but highly endorsed because of its lower than average respiratory depression when compared to other analgesics and neuroprotective properties [8]. Some potential adverse effects are laryngospasm (which normally self resolves), hypertension, and bradycardia in patients with known conduction system pathology.
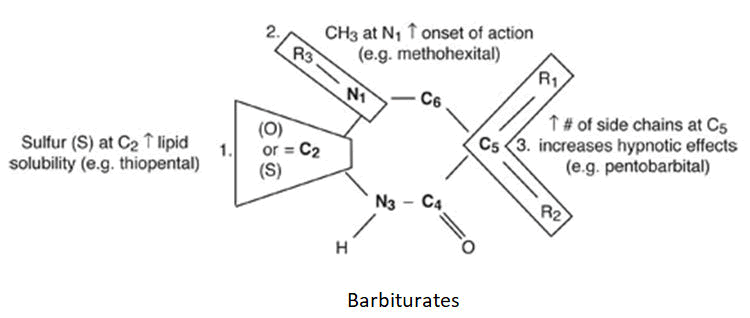
Barbiturates: Pentobarbital is the most frequently used barbiturate in the pediatric population because it is the most efficacious and fewer adverse effects than other barbiturates. Barbiturates fall under the hypnotic category and are excellent source of sedation. Similar to benzodiazepine, they act on the availability of GABA in the brain by interfering with GABA receptors. It can be administered by IV at 1-3 mg/kg and can be repeated every 3-5 minutes as needed with a max dose of 600 mg [9]. For oral dosing it is 3-6 mg/kg with a max dose of 100 mg. Respiratory depressions can occur in up to 11% of pediatric patients, ataxia, prolonged drowsiness, and severe agitation can also occur. Barbiturates should be avoided in patients with known heart conditions, due to their characteristic cardiac depression. Phenobarbital is another barbiturate, but not frequently used for diagnostic imaging sedation purpose, because of even more prolonged sedation.
Results and Discussion
Results from a double blind study, using the Richmond Agitation Sedation Scale (RASS), compared midazolam and chloral hydrate, showed a frequency of light and moderate sedation in the midazolam group at 55.9% and 11.8% respectively, and in the chloral hydrate group it was 50% and 20.6% respectively [10]. Additionally, we found that midazolam was superior in the average time of onset with an average time of 6.35 minutes, and chloral hydrate averaging onset at 19.14 minutes. No respiratory or neurological adverse effects were observed in either group, however gastrointestinal side effects was 0% in the midazolam group and 23.5% in the chloral hydrate group. Plus, in a cohort study done by Stern KW from 2014, the data shows that the average diagnostic error in echocardiograms is 6.5%, and even higher in patients with complicated anatomy that are not sedated. Sedated patients had image quality concerns in 22% whereas non-sedated patients have image quality concerns in 60% of cases. There were 17% less incomplete echocardiogram reports in sedated patients than in non-sedated, further supporting the need for sedation in important imaging studies.
Midazolam ultimately remains superior in effectivity, ease of use and at decreasing diagnostic errors in echocardiograms. Nonetheless, oral midazolam has variable first pass metabolism which causes unpredictable systemic availability, whereas intranasal midazolam has greater systemic bioavailability because it avoids hepatic metabolism. When comparing intranasal administration of midazolam versus dexmedetomidine Miller JW, et al. reported that aerosolized intranasal dexmedetomidine offers satisfactory conditions for TTE in children three months to three years of age administered under the supervision of a pediatric cardiac anesthesiologist; while Lewis J, et al. reviewed published randomized controlled trials that included 14 trials with 1809 patients ranging in age from one month to 14 years. Various sedatives were compared with intranasal dexmedetomidine administered in a dose range of 1-4 g/kg. However, for sedation during a TEE we found that midazolam remained superior with a scan time of 8.84 and 9.18 in dexmedetomidine, respectively. The satisfaction of the sonographer was also better for those receiving midazolam with a satisfactory score of 9.88 and 7.64 in the dexmedetomidine group.
The study done by Warden CN, et al. to determine the efficacy and safety of oral pentobarbital for sedation during pediatric TTE showed an overall sedation success rate as 98.7% in 9796 children, and that of those 99% remained sedated throughout the study. The overall adverse event rate was 0.5%, which is minimal. Young children, however, were more likely to experience adverse events, require second dosages, and ultimately failed sedation. When comparing pentobarbital to chloral hydrate, there were fewer episodes of respiratory depression with PB (0.3% vs. 1.6%, P<0.05), but higher rate of paradoxical reactions was higher with PB (1% vs. 0.03%, P<0.05). Thus, chloral hydrate has increased transient desaturation and pentobarbital had increased paradoxical reaction, essentially equally effective and equally safe for sedation in pediatric transthoracic echocardiography.
In a recent review article by Dong SZ, regarding pediatric patients undergoing an MRI it was found that pediatric patients requiring medical sedation are at risk of both acute and long term effects [11]. We know that with sedatives and hypnotics some of the more common serious side effects are respiratory depression, cardiac arrhythmias and hypotension; however neurotoxicity and long term developmental deficits have also been reported. Studies show that up to 5% of pediatric patients sedated with phenobarbital 2-4 mg/kg experience respiratory depression, commonly with hypoxia and increased risk of aspiration which can lead to secondary pneumonia. It was found that the percentage of patients that suffered respiratory depression and apnea is even higher in those that received midazolam, with 20% of pediatric patients requiring supplemental oxygen.
Considering echocardiograms do not require complete immobilization, like other radiographic imaging, we can infer that feeding and distracting of the patients as two viable options for carrying out a successful exam. In an article regarding procedural sedation recommendations Babu T, it states that in routine echocardiograms sedation is not routinely required. Even in infants and younger children under the age of 4, who are unable to comprehend, these techniques have shown favorable diagnostic outcomes. It is important to note that patients needing an echocardiogram may not always be hemodynamically stable and thus may not tolerate medical sedation. Historically, when feeding infants and toddlers they are more likely to refrain from crying, screaming and even scrambling around. A recent study by Ferrer FS determined that playing cartoons, as form of distraction in children with an average age of 26 months, significantly lowered the amount of time needed to perform an echocardiography by about 22.97%. In a bivariate analysis in the same study, the quality of the echocardiograms was found to be about 20% better in the control group in which cartoons were played during the procedure. Furthermore, because echocardiograms are short procedures one can consider that with good technique and adequate anatomical expertise the necessary pictures and recordings should be feasible without medical sedation. When considering the severe respiratory depression and possible longterm effects, the challenges of achieving optimal echocardiogram results can be seemingly accounted for by other techniques.
An important consideration regarding the use of analgesics and sedatives for diagnostic imaging is the American Academy of Pediatrics guidelines which suggest a need for fasting to prevent vomiting, and protection of patient’s airway reflexes which can cause the patient to aspirate. This confounding factor may play an important role in the child’s behavior and further escalate the patient’s resistance and lack of compliance. In infants, fasting from breast milk consumption for a minimum of four hours presumably will increase the child’s irritableness (Table 1).
| Solid or liquid food | Duration of fast |
|---|---|
| Clear liquids | 2 hours |
| Breast milk | 4 hours |
| Infant formula | 6 hours |
| Solids | 6 to 8 hours |
Table 1: Preprocedure guidelines according american academy.
Conclusion
It is universal that patients under the age of 4 are unable to comprehend and will frequently scream and cry during transthoracic echocardiograms, despite parental reassurance. Although there has been development of new sedatives, intranasal midazolam proves to be the leading contender for achieving adequate sedation and minimizing diagnostic errors. However, feeding, and different forms of distraction, such as cartoons, bubbles, sugar and music have shown compelling results for obtaining a good echocardiogram. Additionally, many parents report feeling anxious and prefer other methods to achieve adequate results. The overall active time needed to conduct the echocardiogram is lower with sedation, but the success rate of completed echocardiograms remains in sedated versus non sedated but distracted patients remains unclear. In the future, a multivariate study analyzing midazolam, other sedatives, and playing cartoons should be investigated to conclude if cartoons, feeding, and comforting the child can withstand the effectiveness and certainty that is achieved through sedation.
References
- Babu A (2013) Procedural sedation in children-what is recommended? Indian Pediatr 50:517-519 [Crossref]
[Google Scholar] [PubMed]
- Dong SZ, Zhu M, Bulas D (2019) Techniques for minimizing sedation in pediatric MRI. J Magn Reson Imaging 50:1047-1054
[Crossref] [Google Scholar] [PubMed]
- Ferrer FS, Murcia MD, Lopez-Pineda A, Ruiz MJ, Beltran DO, et al. (2019) Effects of watching cartoons during an echocardiography on infants and preschool children. A prospective randomized study. Front Pediatr 7:184
[Crossref] [Google Scholar] [PubMed]
- Ganigara M, Srivastava S, Malik P, Fong S, Ko H, et al. (2019) Comparison of chloral hydrate and pentobarbital sedation for pediatric echocardiography. Echocardiography 36:766-769
[Crossref] [Google Scholar] [PubMed]
- Krauss BS, Krauss BA, Green SM (2014) Procedural sedation and analgesia in children. N Engl J Med 370:e23
[Crossref] [Google Scholar] [PubMed]
- Lewis J, Bailey CR (2020) Intranasal dexmedetomidine for sedation in children; A review. J Perioper Pract 30:170-175
[Crossref] [Google Scholar] [PubMed]
- Miller JW, Divanovic AA, Hossain MM, Mahmoud MA, Loepke AW (2016) Dosing and efficacy of intranasal dexmedetomidine sedation for pediatric transthoracic echocardiography: A retrospective study. Can J Anaesth 63:834-841
[Crossref] [Google Scholar] [PubMed]
- Panda S, Pujara J, Chauhan A, Varma A, Venuthurupalli R, et al. (2021) Comparative study of intranasal dexmedetomidine v/s midazolam for sedation of pediatric patients during transthoracic echocardiography. Ann Card Anaesth 24:224-229
[Crossref] [Google Scholar] [PubMed]
- Salehi F, Riasi HR, Ebrahimzadeh A, Askari Janatabadi S (2017) The Effect of Oral Midazolam and Chloral Hydrate Before Echocardiography in Pediatric Patients: A Randomized Double-Blind Clinical Trial. Glob Pediatr Health 4
[Crossref] [Google Scholar] [PubMed]
- Stern KW, Gauvreau K, Geva T, Benavidez OJ (2014) The impact of procedural sedation on diagnostic errors in pediatric echocardiography. J Am Soc Echocardiogr 27:949-955
[Crossref] [Google Scholar] [PubMed]
- Warden CN, Bernard PK, Kimball TR (2010) The efficacy and safety of oral pentobarbital sedation in pediatric echocardiography. J Am Soc Echocardiogram 23:33-37
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
