Pulse Oximeter in the Diagnosis of Neonatal Cardiology Diseases at Birth
Isha Deshmukh*
Department of Pediatrics and Neonatology, University BJ Government Medical College, Pune, India
- *Corresponding Author:
- Isha Deshmukh
Department of Pediatrics and Neonatology,
University BJ Government Medical College,
Pune,
India,
Email: anmoldshmkh.81@gmail.com
Received: May 03, 2021, Manuscript No. IPIPC-23-8356; Editor assigned: May 06, 2021, PreQC No. IPIPC-23-8356 (PQ); Reviewed: May 20, 2021, QC No. IPIPC-23-8356; Revised: November 01, 2023, Manuscript No. IPIPC-23-8356 (R); Published: November 29, 2023, DOI: 10.36648/Insigh Pediatr Card.7.3.262
Citation: Deshmukh I (2023) Pulseoximeter in the Diagnosis of Neonatal Cardiology Diseases at Birth. Insigh Pediatr Card: Vol.07 No.3: 262.
Abstract
Health outcomes are improved when newborn babies with critical congenital heart defects are detected before acute cardiovascular collapse. The main screening tests used to identify these babies include prenatal ultrasound and postnatal clinical examination. However, even though both these methods are available, a significant proportion of babies are still missed. Routine pulse oximeter readings have been reported as an additional screening test that can potentially improve the detection of CCHD. Continuous measurements with the pulse oximeter are very simple and very reliable. Because the Pulseoximeter responds rapid to oxygenation changes and does not need calibration, it is very valuable in the assessment of therapeutic procedures in patients with cyanotic heart diseases. We hereby conclude that the pulse oximeter is an important new diagnostic tool in pediatric cardiology. We reviewed the available literature addressing current detection methods for CCHD, burden of missed and/or delayed diagnosis of CCHD, rationale of oximetry screening, and clinical studies of oximetry in otherwise asymptomatic newborns.
Keywords
Pulseoximeter; Neonatal; Cardiology; Birth
Description
Congenital heart diseases occur in 8 per 1000 live births; with approximately 1/3 of these neonates requiring intervention in the first month of life. Neonates with respiratory distress; cyanosis or dysmorphic syndromes commonly have CHD. Clinical suspicion increase in a symptomatic infant with a cardiac murmur, but the presence or absence of a murmur does not assure either the presence or absence of significant CHD [1-3]. Infants suspected to have CHD may be divided into premature and term infants, as well as infants with duct dependent pulmonary blood flow, infants with duct dependent systemic blood flow, and infants with unrestricted pulmonary blood flow based on pulse-oximetry values.
Many cross sectional studies and retrospective studies used a common screening protocol for diagnosis of congenital heart diseases by simple tool of pulse-oximetry for neonates before discharge.
Timely reliable monitoring is vital when trying to accurately assess a newborn oxygenation status. Sensors provide monitoring solutions specifically for newborns that help clinicians with pertinent physiological data quickly and efficiently without sacrificing accuracy [4-6]. Pulse-oximetry demonstrates the highest sensitivity and specificity during induced conditions of motion and low perfusion.
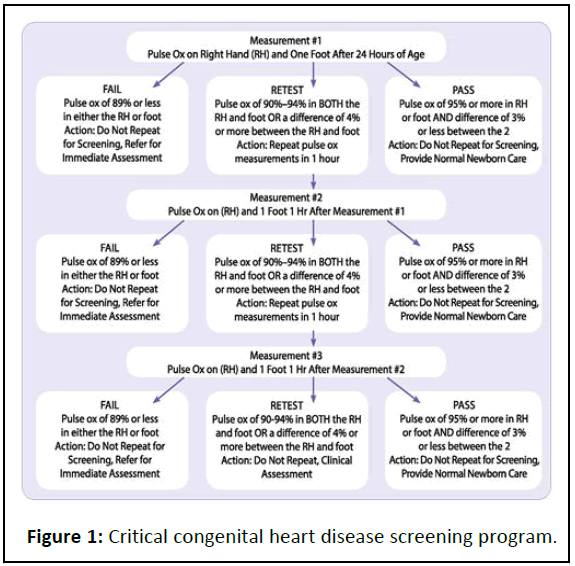
Pulse oximetry estimates arterial oxygen saturation by measuring the absorption of light in human tissue beds. As light passes through human tissue, it is absorbed in various degrees by tissue, bone, blood vessels, fluids, skin, venous and arterial blood, including various types of haemoglobin [7-9]. The light absorption changes as the amount of blood in tissue bed changes and as the relative amount of oxygenated and deoxygenated haemoglobin change[10] (Figure 1).
Failed screen: A screen is considered failed if:
• Any oxygen saturation measure is <90% (in the initial screen or
in repeat screen).
• Oxygen saturation is <95% in the right hand and foot on three
measures, each separated by one hour.
• A saturation >3% difference exists in oxygen saturation
between the right hand and foot on three measures, each
separated by one hour.
Any infant who fails the screen should have an evaluation for causes of hypoxemia. If a reversible cause of hypoxemia is identified and appropriately treated, an echocardiogram may not be necessary.
Passed screens: Any screening with an oxygen saturation measure that is >95% in the right hand or foot with a <3% absolute difference between the right hand and foot is considered a passed screen and screening should end [11-13]. To reduce false positive screens, screen the neonate while baby is alert or after 24 hours old.
Meta-analysis: According to a cross sectional study in term neonates done in July 2010 and April 2011; pulse-oximetry was determined before neonatal hospital discharge and in case of post ductal oxygen saturation <95%, a Doppler Echocardiogram was performed. It was concluded that pulse-oximetry had a good sensitivity and specificity for the identification of CHD in neonates. Low oxygen saturation, higher respiratory frequency and early post-natal age were related to CHD.
An update work done in 2017 of pulse-oximetry screening for detecting critical congenital heart disease in the newborns concluded that pulse-oximetry is safe, feasible and non-invasive method for screening CHD [14,15]. It is a nice method to detect the CHD along-with the physical evaluation by medical personal.
Pulse-oximetry is also used for detection of birth prevalence of critical cyanotic CHD. Studies based on pulse-oximetry for timely diagnosis of CHD helps us to improve survival and reduce morbidity. Hence it would be ideal to identify CHD neonates at birth to initiate appropriate treatment promptly. It is important to classify symptomatic and asymptomatic neonates with cardiac diseases/cardiac emergencies i.e. when they occur and to discuss the underlying pathophysiology.
Conclusion
Diagnosis in the delivery room or nursery includes pulseoximetry, NIBP measures of all 4 limbs, evaluation of central and peripheral pulse status, blood gas evaluation, hyperoxia test and echocardiography in suspected CHD neonates. Collectively, the evidence from our evaluation and meta-analysis supports the easy method, the feasibility, minimal burden and potential benefits of implementing systemic early screening in newborns for identifying congenital heart diseases.
Funding
None.
Conflict of Interest
None.
Acknowledgement
To the head of the department of pediatrics Dr Aarti A Kinikar, BJGMC, Pune who has been supporting and encouraging publications related to neonatology screening. to the dean, Dr Murlidhar Tambe, BJGMC and Sassoon general hospitals, Pune.
References
- Mawson IE, Babu PL, Simpson JM, Fox GF (2018) Pulse oximetry findings in newborns with antenatally diagnosed congenital heart disease. Eur J Pediatr 177: 683-689.
[Crossref] [Google Scholar] [PubMed]
- Mathur NB, Mathur SB (2017) Pulse oximetry screening of neonates for congenital heart disease. Res Cardiovasc Med 6: 1-7.
- Ewer AK, Martin GR (2016) Newborn pulse oximetry screening: Which algorithm is best? Pediatrics 138.
[Crossref] [Google Scholar] [PubMed]
- Bachman TE, Newth CJ, Iyer NP, Ross PA, Khemani RG (2019) Hypoxemic and hyperoxemic likelihood in pulse oximetry ranges: NICU observational study. Arch Dis Child-Fetal Neonatal Ed 104: 274-279.
[Crossref] [Google Scholar] [PubMed]
- Salyer JW (2003) Neonatal and pediatric pulse oximetry. Respir Care 48: 386-398.
[Google Scholar] [PubMed]
- Plana MN, Zamora J, Suresh G, Fernandez-Pineda L, Thangaratinam S, et al. (2018) Pulse oximetry screening for critical congenital heart defects. Cochrane Database Syst Rev 3: CD011912.
[Crossref] [Google Scholar] [PubMed]
- van Naarden Braun K, Grazel R, Koppel R, Lakshminrusimha S, Lohr J, et al. (2017) Evaluation of critical congenital heart defects screening using pulse oximetry in the neonatal intensive care unit. J Perinatol 37: 1117-1123.
[Crossref] [Google Scholar] [PubMed]
- Goetz EM, Magnuson KM, Eickhoff JC, Porte MA, Hokanson JS (2016) Pulse oximetry screening for critical congenital heart disease in the neonatal intensive care unit. J Perinatol 36: 52-56.
[Crossref] [Google Scholar] [PubMed]
- Narayen IC, Blom NA, van Geloven N, Blankman EI, van den Broek AJ, et al. (2018) Accuracy of pulse oximetry screening for critical congenital heart defects after home birth and early postnatal discharge. J Pediatr 197: 29-35.
- Hu XJ, Zhao QM, Ma XJ, Yan WL, Ge XL, et al. (2016) Pulse oximetry could significantly enhance the early detection of critical congenital heart disease in neonatal intensive care units. Acta Paediatr 105: 499-505.
[Crossref] [Google Scholar] [PubMed]
- Ewer AK (2014) Pulse oximetry screening for critical congenital heart defects in newborn infants: Should it be routine? Arch Dis Child-Fetal Neonatal Ed 99: 93-95.
[Crossref] [Google Scholar] [PubMed]
- Ewer AK (2016) Screening for critical congenital heart defects with pulse oximetry: Medical aspects. Am J Perinatol 33: 1062-1066.
[Crossref] [Google Scholar] [PubMed]
- Manja V, Mathew B, Carrion V, Lakshminrusimha S (2015) Critical congenital heart disease screening by pulse oximetry in a neonatal intensive care unit. J Perinatol 35: 67-71.
[Crossref] [Google Scholar] [PubMed]
- Narayen IC, Blom NA, Ewer AK, Vento M, Manzoni P, et al. (2016) Aspects of pulse oximetry screening for critical congenital heart defects: when, how and why? Arch Dis Child-Fetal Neonatal Ed 101: 162-167.
[Crossref] [Google Scholar] [PubMed]
- Harden BW, Martin GR, Bradshaw EA (2013) False-negative pulse oximetry screening for critical congenital heart disease: The case for parent education. Pediatr Cardiol 34: 1736-1738.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences