Long RP Tachycardia in a Toddler with Dilated Cardiomyopathy: What is the Mechanism?
Gonzalez Corcia M Cecilia, Akila Bersali and Christophe Scavee
1Department of Pediatric Cardiology, Cliniques Universitaires St-Luc, Université Catholique de Louvain,Brussels, Belgium
2Department of Cardiology, Cliniques Universitaires St-Luc, Université Catholique de Louvai, Brussels, Belgium
- Corresponding Author:
- Gonzalez Corcia M Cecilia
Department of Pediatric Cardiology Cliniques Universitaires St-Luc
Université Catholique de Louvain
Avenue Hippocrate 10 B-1200 Brussels, Belgium
Tel: +32 474 483 664
E-mail: maria.c.gonzalez@uclouvain.be
Received Date: August 04, 2016; Accepted Date: August 23, 2016;Published Date: September 28, 2016
Citation: Cecilia GCM, Bersali A, Scavée C.Long RP Tachycardia in a Toddler with Dilated Cardiomyopathy: What is the Mechanism?. Insights Pediatr Cardiol 2016, 1:1.
Abstract
The article presents a case of a toddler with incessant supraventricular tachycardia and severe hearth failure confirmed by transthoracic echocardiography. Adenosine administration briefly terminated the arrhythmia for a couple of beats and the tracings recorded during this test allowed to make a precise clinical diagnosis of the type of arrhythmia. Medical therapy failed to controlled the arrhythmia, and the child underwent a percutaneous catheter ablation which successfully terminated with the tachycardia. Taking as a model this unusual pediatric case, the article discusses the most frequent supraventricular arrhythmias in children and gives clues for a precise non-invasive diagnosis.
Keywords
Incessant SVT; Tachycardia-induced cardiomyopathy; Permanent junctional reciprocating tachycardia; Ectopic atrial tachycardia; Pediatric ablation
Case Presentation
A healthy 2-year old boy was referred to our center because of increased heart rate of 190-200 beats per minute, discovered during a regular pediatric visit. At clinic examination, he presented with normal respiratory rate and discrete hepatomegaly of 1cm below the rib cage. The child was previously healthy with no prenatal or post-natal history. At admission, a transthoracic echocardiography demonstrated normal anatomy but a decreased left ventricular ejection fraction of 30%. A 12 lead electrocardiogram (ECG) showed an incessant long RP tachycardia (Figure 1A). An intravenous catheter was placed and a dose of adenosine 0.1 mg/kg (1 mg for 10 kilograms of body weight) was administered by a rapid intravenous. The adenosine terminated the tachycardia to sinus rhythm for a minute, but the initial tachycardia re-started reproducing the initial rates and ECG patterns. The patient was admitted under continuous monitoring and started initially on sotalol (10 mg TID), which resulted in a decrease in the heart rate from180 to 160, but did not stop the tachycardia. After 48 hours, flecainide (10 mg TID) was added with no change in the heart rate. Given the incessant tachycardia with persistence of heart dysfunction, an electrophysiology study was performed with a plan for catheter ablation. The sotalol and flecainide were stopped 48 hours before the study rate control was attempted by oral propranolol.
Figure 1: (A) Twelve-leads surface electrocardiogram showing a narrow complex tachycardia at a rate of 175bpm, with a long RP interval and negative P waves in the inferior leads and left precordial leads. (B) A dose of intravenous adenosine results in atrioventricular block and termination of the tachycardia. The sinus rhythm overtakes with initial 2:1 blocked. (C) Sinus tachycardia at the right end of the tracing.
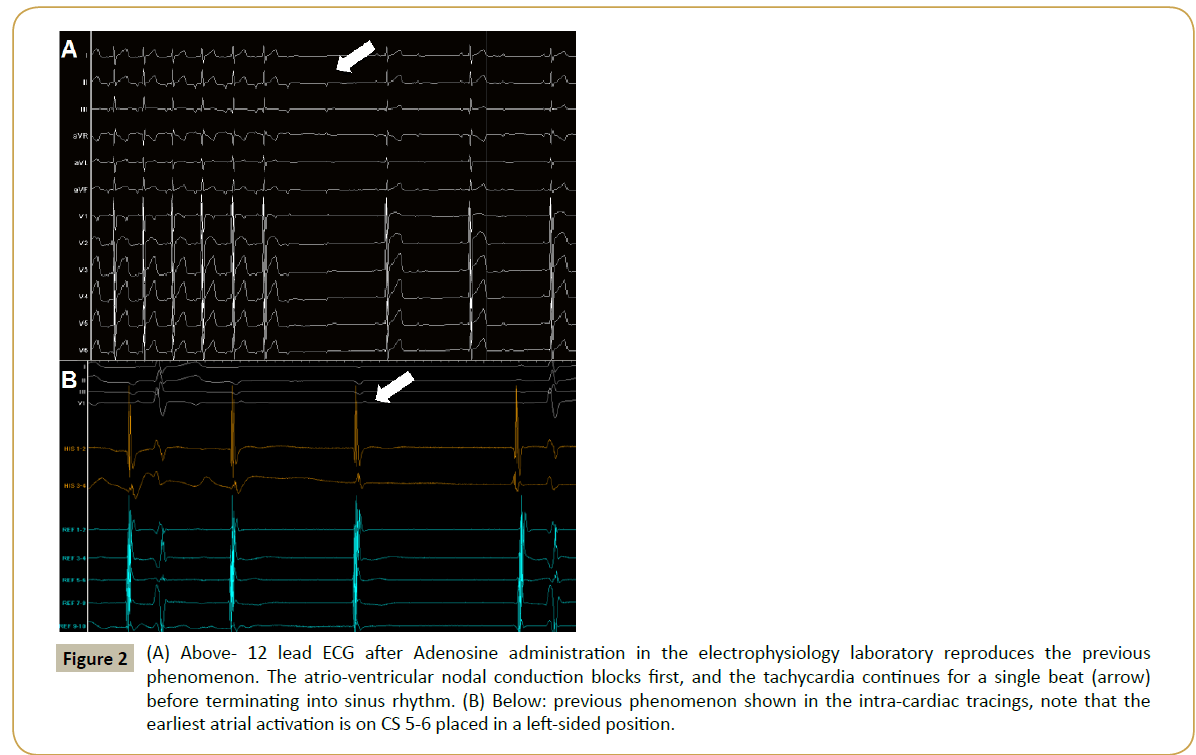
At the beginning of the study, the patient was in incessant long RP tachycardia at a rate of 170 bpm. Access was gained via the right and left femoral veins (6Fr and 7Fr). A decapolar catheter was placed in the coronary sinus and a quadripolar catheter was used to identify the His position. A new dose of Adenosine during tachycardia reproduced the previous phenomenon of initial atrioventricular block, followed by a termination of the tachycardia after a single atrial beat (Figure 2A). Note that during tachycardia, the intra-cardiac recordings show the earliest atrial activation in the left proximal-to-mid coronary sinus. Re-initiation of the tachycardia occurred after 10 seconds of sinus rhythm. The initial P wave of the tachycardia was identical to all subsequent P waves. Moreover, paced ventricular extra stimuli, timed to His bundle refractoriness, were administered from the right ventricular apex with no change in the timing of the atrial electrogram.
Figure 2: (A) Above- 12 lead ECG after Adenosine administration in the electrophysiology laboratory reproduces the previous phenomenon. The atrio-ventricular nodal conduction blocks first, and the tachycardia continues for a single beat (arrow) before terminating into sinus rhythm. (B) Below: previous phenomenon shown in the intra-cardiac tracings, note that the earliest atrial activation is on CS 5-6 placed in a left-sided position.
On the basis of these findings, a diagnosis of a rare form of left atrium incessant ectopic atrial tachycardia responsive to adenosine was easily made. A trans-septal puncture was performed under fluoroscopic and trans-oesophagic guidance without complications. The left atrium was carefully mapped and the earliest atrial signals were identified in the posterior region of the mitral valve annulus. An initial radiofrequency ablation at a relatively low power (30W) resulted in tachycardia termination within 2 seconds and resumption of sinus rhythm (Figure 3). One month after the ablation, the patient had completely normalized the heart function.
Figure 3: (A) LAO view during transeptal puncture. Note the position of the long sheath and the presence of the trans-oesophageal probe. (B) LAO view showing catheter position at site of success at the left postero-to-mid septal region. (C) Intracardiac electrograms during successful ablation. Note the signals at site of success with presence of sharp atrial pre-potential. Following onset of radiofrequency ablation the tachycardia terminated into sinus rhythm within 2 seconds.
Discussion
Narrow complex tachycardia with a long RP interval (RP interval ≥ PR interval) includes 3 differential diagnoses at any age:
1.Atypical form of AV nodal reentrant tachycardia (AVNRT).
2.Orthodromic AV reciprocating tachycardia (ORT), most probably using a slow conducting decremental concealed postero-septal accessory pathway.
3.Atrial tachycardia.
Given the age of the patient, the ECG pattern and response to adenosine, and the incessant arrhythmia resulting in cardiomyopathy, the most probable diagnosis in our patient would be Permanent Junctional Reciprocating Tachycardia (PJRT). PJRT is the most frequent form of long RP tachycardia in young children with tachycardia-induced cardiomyopathy [1]. PJRT or atrioventricular reentrant tachycardia utilizing a slowly conducting posteroseptal accessory pathway is a rare form of reentrant supraventricular tachycardia. The characteristic features of this narrow complex tachycardia are a long RP interval, inverted P waves in the inferior leads and termination by adenosine. This form of accessory-pathway-mediated tachycardia, which is usually incessant, can lead to a tachycardia-induced cardiomyopathy and congestive heart failure if left untreated [2,3].
However, in our patient, PJRT could have been already ruled out at admission as the clue about mechanistic diagnosis was present in the initial adenosine test (Figure I). A vigilant electro physiologist would have noticed that the tachycardia continued for a single beat after atrio-ventricular nodal conduction blocked, ruling out a re-entrant mechanism. Even more rare, automatic atrial tachycardia originating from the left atrium have been described as cause of incessant tachycardia associated to left ventricular dysfunction at a young age [4].
Ectopic atrial tachycardia (EAT) is an automatic tachycardia originating from the atrium [5,6]. Incessant EAT can cause ventricular dysfunction and cardiomyopathy [7]. Catheter ablation in young children is indicated for incessant tachycardia, tachycardia induced cardiomyopathy, or paroxysmal tachycardia that has not responded to combination medications. The rarity of our case resides both in the clinical presentation with a response to adenosine that could misguide the initial diagnoses and in the rarity of mitral locations in this age group of article.
References
- Vaksmann G, D'Hoinne C, Lucet V, Guillaumont S, Lupoglazoff JM, et al. (2006) Permanent junctional reciprocating tachycardia in children: a multicentre study on clinical profile and outcome. Heart 92:101-104.
- Bensler JM, Frank CM, Razavi M, Rasekh A, Saeed M, et al. (2010) Tachycardia-Mediated Cardiomyopathy and the Permanent Form of Junctional Reciprocating Tachycardia. Tex Heart Inst J 37:695-698.
- Kang KT, Potts JE, Radbill AE, La Page MJ, Papagiannis J, et al. (2014) Permanent junctional reciprocating tachycardia in children: A multicenter experience. Heart Rhythm 11:1426-1432.
- Bonney W, Shah M (2013) Incessant SVT in children: Ectopic atrial tachycardia and permanent junctional reciprocating tachycardia. Progress in Pediatric Cardiology35:33-40.
- Toyohara K, Fukuhara H, Yoshimoto J, Ozaki N, Nakamura Y (2011)Electrophysiologic studies and radiofrequency catheter ablation of ectopic atrial tachycardia in children. PediatrCardiol32:40-46.
- Ge H, Li X, Zhang Y, Liu H, Jiang H (2015) Clinical course and treatment of ectopic atrial tachycardia in 144 children. ZhonghuaErKeZaZhi53:214-219.
- Mehta AV, Sanchez GR, Sacks EJ, Casta A, Dunn JM, et al. (1988) Ectopic automatic atrial tachycardia in children: clinical characteristics, management and follow-up. J Am CollCardiol11:379-385.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences